by Frederike Buhse, Exzellenzcluster Präzisionsmedizin für chronische Entzündungserkrankungen
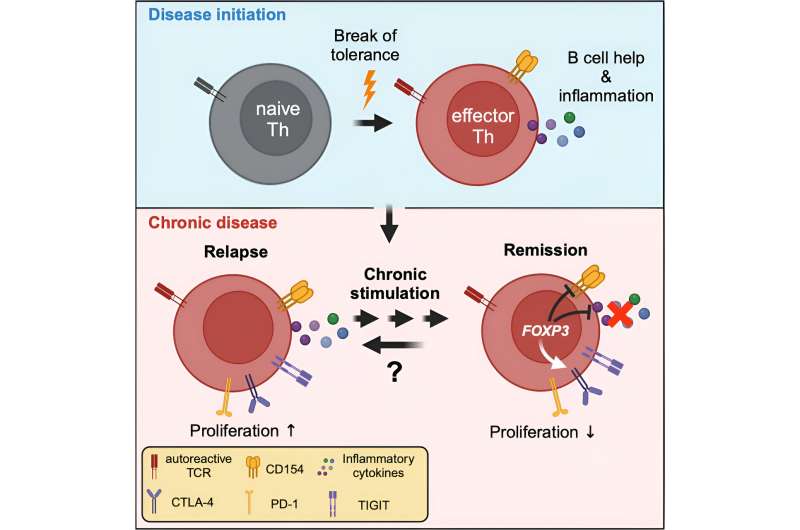
Graphical abstract. Credit: Immunity (2024). DOI: 10.1016/j.immuni.2024.08.005
In autoimmune diseases, the immune system mistakenly attacks the body’s own structures. A research team from Kiel, Lübeck and Berlin has now succeeded in analyzing certain pathogenic immune cells more precisely using a method they developed.
They discovered that these cells can sometimes switch to a dormant (“exhausted”) state for years, making them inaccessible to existing therapeutic approaches. If the cells then switch back to an active state, they trigger further immune cells to attack the body’s own structures and thus reignite the disease.
The interdisciplinary research team, which included numerous members of the Cluster of Excellence “Precision Medicine in Chronic Inflammation” (PMI), recently published its findings in Immunity.
Autoreactive immune cells in a dormant state
The researchers examined blood samples from patients who had one of three autoimmune diseases in which the structures against which the immune system is directed are known. Using a method they developed (antigen-reactive T cell enrichment, ARTE), they were able to selectively enrich and analyze the rare autoreactive immune cells from the large number of different immune cells in the blood. These are the cells that react incorrectly to the body’s own structures, trigger inflammation and cause other immune cells to attack the body’s own structures.
“Until now, it was assumed that these cells are chronically activated in autoimmune diseases and thus drive the inflammation,” explained first author Dr. Carina Saggau from the Institute of Immunology at Kiel University and the University Medical Center Schleswig-Holstein (UKSH), Kiel Campus.
“But we have now been able to show that, surprisingly, some of them are in a dormant state, known in science as ‘exhausted,’ and in some cases circulate in the blood in this state for years.” This dormant state is known from tumor research: In tumors, the immune cells that should actually be fighting the tumor are in such a state and therefore allow the tumor to grow unhindered.
“In the autoimmune diseases we are investigating, we suspect that the chronic activation by the body’s own structure leads to a kind of ’emergency shutdown’ after a while. The body needs a mechanism to switch off cells that are permanently activated,” says Professor Alexander Scheffold, Director of the Institute of Immunology and member of the Cluster of Excellence ‘Precision Medicine in Chronic Inflammation’ PMI.
The immunologist led the interdisciplinary research work together with neuroimmunologist PD Frank Leypoldt from the Institute of Clinical Chemistry at the UKSH, Kiel Campus, and Professor Friedemann Paul from the Experimental and Clinical Research Center at Charité, Berlin.
Reactivation of dormant cells leads to new disease flare-ups
In autoimmune diseases, however, the dormant state also means that these cells escape the usual therapies aimed at suppressing the overreactive immune system. This means that the therapy often works and suppresses the symptoms of the autoimmune reaction, but some of the pathogenic T cells survive in the dormant state. If some of the dormant cells are reactivated, presumably by infections or environmental factors, they can switch the entire disease process back on. Those affected experience a new flare-up of the disease.
“This observation explains why current therapies do not offer lasting protection against relapses,” explains PD Frank Leypoldt, also a member of the PMI Cluster of Excellence. “At the same time, they open up new approaches for more targeted therapies. For example, we could try to selectively attack the dormant cells with therapies specifically aimed at them and thus treat the disease more effectively, sustainably and precisely. Alternatively, based on existing approaches from tumor medicine, the cells could be reactivated in order to better target them therapeutically.”
The observations are also important for a better understanding of the underlying disease mechanisms, emphasizes Scheffold. “We have now shown the connections for the first time in three model diseases. Next, we would like to investigate in which other inflammatory diseases we find this condition in order to better understand what underlies the various diseases. This is the only way to enable specific treatment of the respective causes of the disease in the sense of true precision medicine,” explains Scheffold.
About the ARTE method
In a blood sample, only about one in a hundred thousand T cells react against the specific autoantigen (i.e., the body’s own molecule against which the immune system is directed in autoimmune diseases). Prof. Petra Bacher and Prof. Alexander Scheffold from the PMI Cluster of Excellence have developed the so-called “antigen-reactive T cell enrichment” (ARTE) in order to be able to study these rare cells at all.
The method is based on briefly exposing blood cells to the antigen in a test tube. Antigen-specific T cells are thus activated and can be labeled with magnetic particles using “activation markers”. Using magnetic separation columns, these rare T cells are then filtered out of a larger amount of blood and analyzed.
More information:
Carina Saggau et al, Autoantigen-specific CD4+ T cells acquire an exhausted phenotype and persist in human antigen-specific autoimmune diseases, Immunity (2024). DOI: 10.1016/j.immuni.2024.08.005
Provided by
Exzellenzcluster Präzisionsmedizin für chronische Entzündungserkrankungen
Citation:
Autoimmune disease researchers find immune cells escape therapy due to ‘exhausted’ state (2024, September 5)
retrieved 13 September 2024
from https://medicalxpress.com/news/2024-09-autoimmune-disease-immune-cells-therapy.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.
Note: This article have been indexed to our site. We do not claim legitimacy, ownership or copyright of any of the content above. To see the article at original source Click Here











.jpg)

